- Research
- Open access
- Published:
Sociodemographic disadvantage in the burden of stress and academic performance in medical school: implications for diversity in medicine
BMC Medical Education volume 24, Article number: 348 (2024)
Abstract
Background
Nontraditional students bring to medicine inherent characteristics and perspectives that enrich the learning environment and contribute to expanding diversity in medicine. However, research has shown that these students, by virtue of their sociodemographic backgrounds, face unique challenges in medical education, which ultimately place them at a disadvantage compared to their peers. The purpose of this study is to explore relationships between sociodemographic characteristics, stress, and academic performance, in the context of outcomes that may be undermining efforts to diversify the physician workforce.
Methods
Using a retrospective observational cohort methodology, we examined institutional and USMLE exam performance data in conjunction with Perceived Stress Scale-4 survey results from six cohorts of students at Kirk Kerkorian School of Medicine at UNLV (n = 358). Using independent samples t-test, mean stress and academic performance were compared between four sociodemographic groups: first-generation college students, underrepresented in medicine (URM), socioeconomically disadvantaged, and age 30 + at matriculation. Results were considered significant where P ≤ .05.
Results
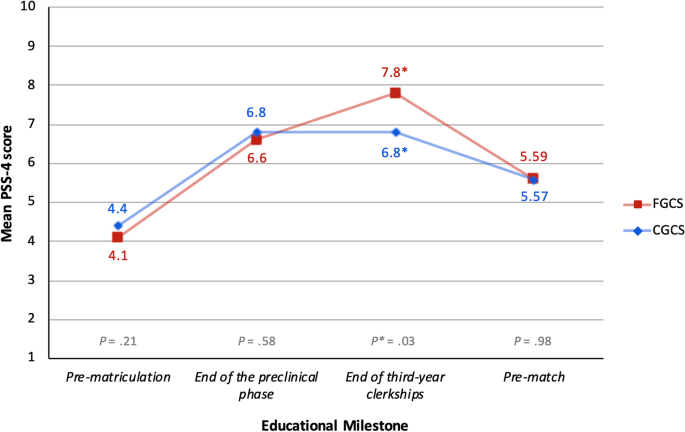
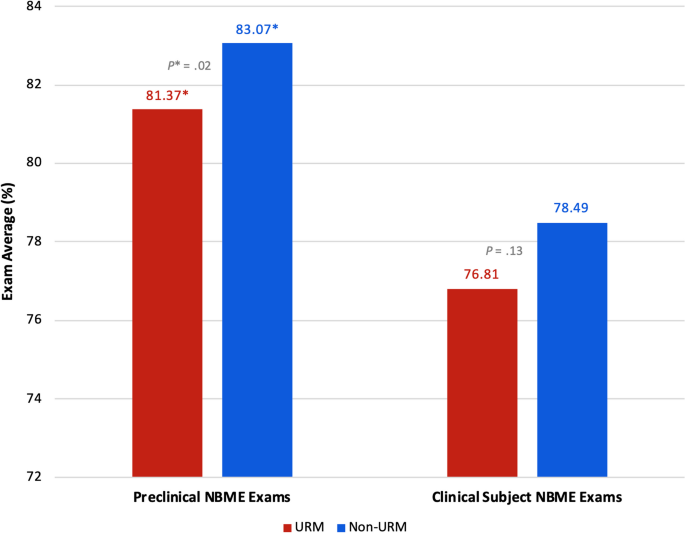
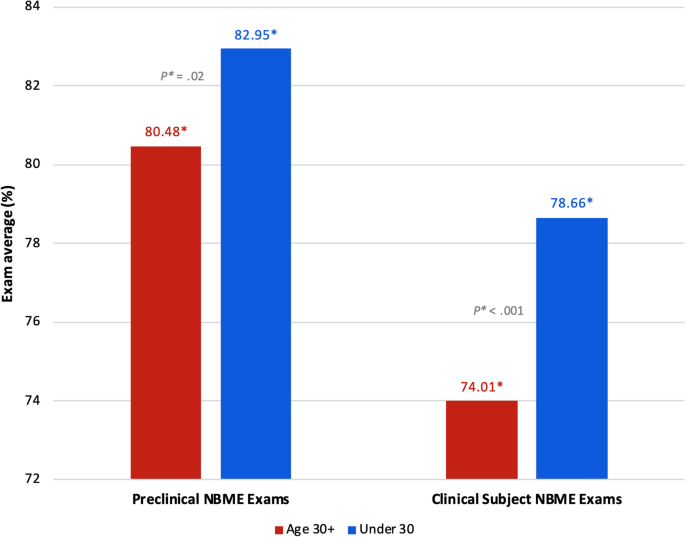
First-generation college students had significantly higher stress at the end of third year clerkships (mean 7.8 vs. 6.8, P* = .03). URM students had significantly lower scores on preclinical exams (mean 81.37 vs. 83.07, P* = .02). The students who were age 30 + at matriculation had significantly lower exam scores on all academic performance measures.
Conclusion
Our results echo historic trends in academic performance for racial and ethnic minority students, and we present recent evidence of academic performance disparities based on age at matriculation. Residency program directors continue to use test scores as a primary metric to screen applicants and thus, poor academic performance has profound consequences on career trajectory. Finally, significantly higher stress in the first-generation students may be evidence of underlying psychological distress. Expanding the sociodemographic diversity among physicians, and by extension, medical students, has long been recognized as fundamental to addressing inequities in healthcare. However, results from our study suggest that aspects of medical education are unfavorable and disadvantageous for first-generation, URM, and older medical students. A deeper understanding of the interplay between sociodemographic characteristics and success in medical school is paramount as we pursue diversity in medicine.
Background
Research has shown that being a medical student is associated with a greater degree of perceived stress, reduced overall wellbeing [1,2,3], higher rates of depression, anxiety, and burnout [4,5,6,7] and that these experiences can negatively impact academic performance [1,2,3, 8]. The 2022 National College Health Assessment (NCHA) survey, which collects data on factors that students perceive to affect their academic performance, reported that the top three factors cited by graduate and professional students were stress (33%), anxiety (28%), and depression (20%) [8]. Common sources of stress in medical education include assessment-related performance pressure, excessive workload, conflicts in school-life balance and personal relationships, peer relations, health concerns, the learning environment, and administrative failures [6, 7, 9,10,11]. In addition to these stressors faced by all medical students, nontraditional studentsFootnote 1 face additional stressors that further compromise health and well-being, detract from academic success, and diminish sense of fulfillment with medical training [1,2,3, 10, 12,13,14,15].
In a study of 69,722 students from more than 100 different U.S. post-secondary institutions, Stevens, et. al. (2018), found that discrimination is a common stressor for racial/ethnic minority undergraduate students, and that these experiences negatively impact their academic performance [16]. These students are also vulnerable to “minority status stress,” which refers to heightened feelings of not belonging that interfere with social integration [17]. Research on older medical students, though sparse, suggests that these students experience a greater overall stress burden due to additional responsibilities outside of medical school and that these responsibilities interfere with studying [18]. Mason et. al. (2018) looked at several indicators of well-being in first-generation medical students. They found significant negative correlations between perceived stress and quality of life across physical, psychological, social, and environmental domains [15]. Studies have shown that financial stress related to excess education debt disproportionately affects racial and ethnic minority, low-income, and first-generation college students [13, 19]. Furthermore, studies show that the accumulation of large amounts of debt during medical school is associated with increased stress [1, 13], poorer academic performance [1], increased risk for burnout [5], and pursuit of higher-paying subspecialties [1, 20].
Nontraditional students bring to medicine inherent characteristics and perspectives that enrich the learning environment [21] and contribute to expanding sociodemographic diversity among physicians [22,23,24]. However, by virtue of their sociodemographic backgrounds, these students face unique challenges in medical education, which ultimately places them at a disadvantage compared to their peers. The purpose of this study is to explore relationships between sociodemographic characteristics, stress, and academic performance, in the context of outcomes that may be undermining efforts to diversify the physician workforce. Utilizing data collected at Kirk Kerkorian School of Medicine at UNLV, we evaluated stress and academic performance in four categories of nontraditional students with the hypothesis that, when compared to their counterparts, these students would have higher perceived stress, lower academic performance, and possibly both. This study will contribute to the growing body of knowledge on stress and academic performance in medical education for those who approach medical school from a place of sociodemographic disadvantage. To the best of our knowledge, this study is among the first to look at stress, at multiple predetermined points in the curriculum, juxtaposed with academic performance. Notably, we report findings on “older” students, a small but richly diverse subset of nontraditional medical students on which research is considerably lacking.
Methods
Sociodemographic characteristics, Perceived Stress Scale-4 (PSS) scores, and exam performance data on 358 of 360 students who matriculated to the Kirk Kerkorian School of Medicine as part of the graduating classes of 2021 through 2026 were utilized for the purposes of this retrospective observational cohort study. Due to substantial fluctuations in graduation timelines, 2 students were not included in any of the data analyses. All study participant data were deidentified prior to retrieval and utilized in accordance with existing IRB-approved protocols. The sociodemographic groups, data, and respective analyses are described below.
Sociodemographic group classification and justification
Selection of nontraditional sociodemographic groups
Using data collected at the time of admission, students were sorted into one or more of the following demographic groups: First-Generation College Student (FGCS), Underrepresented in Medicine (URM), Socioeconomically Disadvantaged (SED), and Age 30 years or older (Age 30 +) at matriculation. These groups were chosen based on data published by the Association of American Medical Colleges (AAMC) showing that these groups are currently underrepresented among medical students. Nationally, of the medical school matriculants in 2022, 11.2% were first-generation college students [25], 22.7% were URM [26], 21.5% were socioeconomically disadvantaged [27], and 5.7% were 29 years of age or older [28]. Furthermore, a 2017 analysis of socioeconomic diversity among US medical students found that, in 2017, 24% of matriculants reported parental income in the top 5% (greater than $225,251) of all US households and over half were from households in the top 20% (greater than $121,019), findings that have been consistent for the past 30 years [29]. Based on these data, we considered these categories (e.g., FGCS, URM, SED, and Age 30 +) to be appropriate nontraditional sociodemographic groups to be included in our study.
First-Generation College Students: FGCS vs. CGCS
Following the AAMC definition, students whose “most highly educated parent/guardian has up to the equivalent of some college but earned no degree” were included in the “FGCS” group. These students were compared to continuing-generation college students (“CGCS”) [25].
Underrepresented in Medicine: URM vs. non-URM
The AAMC defines underrepresented in medicine (URM) as “racial and ethnic populations that are under-represented in the medical profession relative to their numbers in the general population" [30]. This definition is purposefully vague with regards to race and ethnicity to allow for geographic differences and/or temporal changes in population diversity. Students who self-selected “Black/African American”, “Hispanic/Latinx”, and “Native American” (e.g., American Indian, Hawaiian Native, or Alaskan Native) were included in the “URM” group; all other race and ethnic groups were included in the “non-URM group”.
Socioeconomic Disadvantage: SED vs. non-SED
Socioeconomic advantage or disadvantage is identified in medical school applicants by combining conventional socioeconomic status (SES) metrics (e.g., annual household income) with additional information regarding parental education and occupation (EO); together, these metrics are known as SES-EO categories, and are stratified into quintiles [29]. Students from households with an annual income below $45,600, or whose parents have “less than a bachelor’s degree, or parents with any degree and a service, clerical, skilled, or unskilled occupation” are classified as SES-EO 1 or 2 and are considered SES-EO disadvantaged. Students from households with annual income above $45,601 or with at least 1 parent with “a bachelor’s degree or higher, and an executive, managerial, or professional occupation” are grouped into EO-3, EO-4, or EO-5 [29]. Our study group “SED” includes SES-EO 1 and 2 students. Students in SES-EO 3, 4, and 5 categories served as the comparison group “non-SED”.
Age at matriculation: age 30 + vs. under 30
To look at differences based on age, we compared students who were 30 years of age or older (“age 30 + ”) to those who were 29 years or younger (“under 30”) at the time of matriculation to medical school. Data from the 2022 AAMC Matriculating Student Questionnaire (MSQ) showed that the vast majority of matriculants were 25 years of age or less (82.9%) [28]. Using this as a reference point, we deemed 30 years of age to be sufficiently different from the average, and thus an appropriate cutoff to represent an “older” medical student.
Stress data
Perceived stress scale-4
As part of continuous internal quality improvement efforts, institutional program evaluation data has been collected from all students beginning in 2017 with the matriculation of the inaugural class at Kirk Kerkorian School of Medicine at UNLV. Part of this evaluation includes assessing student stress using the Short Form Perceived Stress Scale Questionnaire (PSS-4), a widely used tool to quantify perceived general stress [28, 31,32,33]. The PSS-4 consists of four questions designed to measure perceived stress over the previous month (see Appendix 1 for an outline of the survey). Each item is scored on a scale of 0 (very low stress) to 4 (very high stress), and the cumulative score out of 16 correlates with the degree of perceived stress [31, 32]. PSS-4 surveys are collected at four educational milestones: (1) prior to matriculation (“pre-matriculation”), (2) at the end of the preclinical phase, (3) at the end of third-year clerkship rotations, and (4) immediately before students participate in the residency matching program (“pre-match”). Due to the rolling nature of program evaluation data collection, all students had not participated in data collection at all educational milestones at the time of the study. For example, all 358 students included in the study had completed the pre-matriculation survey, while only 139 students had completed the pre-match survey.
Academic performance data
Institutional NBME exam performance: “preclinical exam average” and "clinical subject exam average”
In the preclinical, organ-systems-based curriculum, student knowledge is assessed using the Customized Assessment Service from the National Board of Medical Examiners (NBME). Each organ-system block varies slightly in length, and, due to evolving curricular structure, each cohort of students have taken a different number of preclinical assessments. For the purposes of comparing academic performance, an average exam score was calculated for each study participant using their scores on all administered preclinical exams. This average exam score for each study participant was then used in the statistical analysis. The results of this analysis are reported as “preclinical exam average”.
Clinical knowledge is assessed during the third year of medical school using Clinical Subject NBME Exams, covering six core specialties (e.g., Internal Medicine, Family Medicine, Pediatrics, Obstetrics and Gynecology, Surgery, and Psychiatry). As described for the preclinical exams, the average exam score calculated for each study participant was used in the statistical analysis. The results of this analysis are reported as “clinical subject exam average”.
USMLE performance: “Step 1” and “Step 2 CK”
Three-digit numeric scores on the Step 1 and Step 2 CK United States Medical Licensing Examinations (USMLE) for each study participant were used in the statistical analysis. Students sit for Step 1 after the preclinical phase and must pass the exam before being promoted to the clinical phase of the curriculum. Students may sit for Step 2 CK at any time after Step 1. Therefore, at the time of this study, some students may have taken none, one, or both USMLE exams. Additionally, we did not include students who took the USMLE Step 1 after January 26, 2022, when the exam moved to Pass/Fail score reporting. Results of this statistical analysis are reported as “Step 1 average” and “Step 2 CK average”.
Statistical analysis
Using these preexisting data sets, independent samples t-tests were calculated with Statistical Package for Social Sciences (SPSS) (version 27) software to assess for differences in PSS-4 scores and academic performance between FGCS vs. CGCS; URM vs. non-URM; SED vs. non-SED; and Age 30 + vs. Under 30. Results were considered significant (indicated as P*) for two-sided P values where P ≤ 0.05. All P values are reported with equal variances assumed unless otherwise noted.
Results
Of the 358 students included in the study, nearly all of them (97.2%) fall into at least one of our nontraditional sociodemographic groups (Table 1).
FGCS vs. continuing-generation college students (CGCS)
Compared to their CGCS peers, we found that FGCS had lower stress at the first two educational milestones (e.g., pre-matriculation and the end of the preclinical phase), roughly the same stress at the final educational milestone (e.g., as students approached the residency match), but, between these points, at the end of third-year clerkships, stress among the FGCS was significantly higher than that of their CGCS counterparts (mean 7.8 vs. 6.8; 95% CI [0.09 to 1.98], P* = 0.03) (Fig. 1; see also Supplementary Table 1, Appendix 2). While the FGCS and CGCS performed roughly the same on the preclinical institutional exams, the FGCS had lower average scores on all other academic performance measures. However, none of these differences met statistical significance (Table 2).
Results of mean PSS-4 score comparison between FGCS vs. CGCS. While actual scores can range from 0 to 16, the y-axis has been amended to a range of 1 to 10 in order to visually present the data. Abbreviations: FGCS first-generation college student, CGCS continuing-generation college student, PSS-4 Perceived Stress Scale-4
Underrepresented in Medicine (URM) vs. non-URM
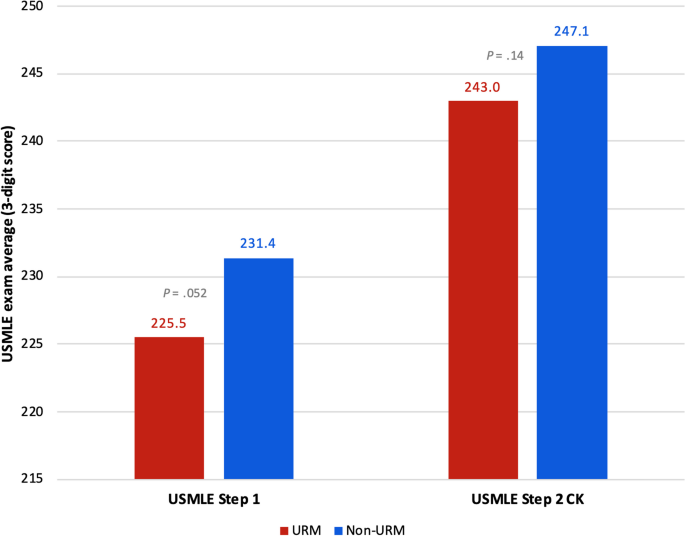
The comparison of stress between URM and non-URM students showed that URM students had lower stress at each educational milestone until the last PSS-4 survey collection, immediately before students participate in the residency match (“pre-match”). However, none of the differences in stress between URM and non-URM students met statistical significance (Table 3). When we compared academic performance, we found that URM students had lower average exam scores on institutional and USMLE exams; however, the only statistically significant difference was performance on the preclinical NBME exams (mean 81.37 vs. 83.07; 95% CI [-3.17 to -0.23], P* = 0.02) (Figs. 2 and 3; see also Supplementary Table 2, Appendix 2).
Results of institutional preclinical and clinical subject NBME exam performance between URM vs. non-URM students. While actual scores can range from 0 to 100, the y-axis has been amended to a range of 72 to 84 in order to visually present the data. Abbreviations: URM underrepresented in medicine, NBME National Board of Medical Examiners
Socioeconomic Disadvantage (SED) vs. non-SED
Socioeconomically disadvantaged (SED) students had higher stress at the first three educational milestones (e.g., pre-matriculation, the end of the preclinical phase, and the end of third-year clerkships) (Table 4), and lower average performance on the clinical subject and USMLE Step 1 exams (Table 5) compared to their non-SED counterparts. However, these differences were not statistically significant.
Age 30 + at matriculation vs. under 30
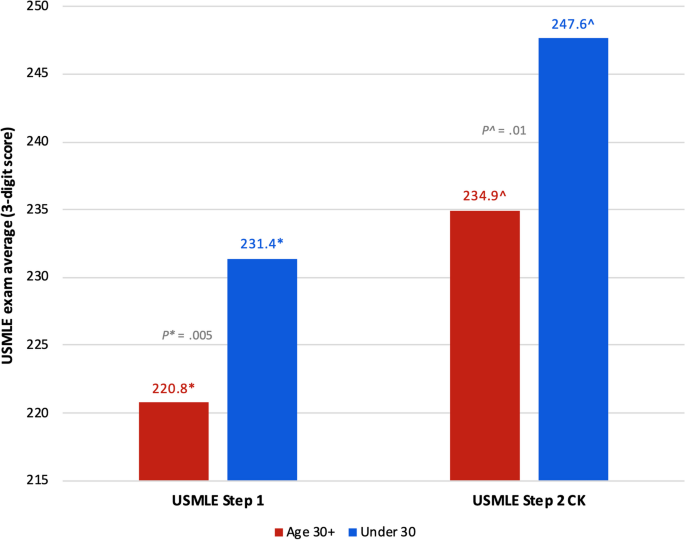
The comparison of stress between the Age 30 + and Under 30 students revealed lower stress among the Age 30 + cohort at the first three educational milestones, and higher stress only before the residency match (Table 6); however, none of these differences were statistically significant. When we compared academic performance between these two groups, the Age 30 + students had significantly lower average exam scores across all academic performance measures (Figs. 4 and 5; see also Supplementary Table 3, Appendix 2). Results of institutional exam performance are shown in Fig. 4, with students who were Age 30 + at matriculation scoring significantly lower on the preclinical exams (mean 80.48 vs. 82.95; 95% CI [-4.52 to -0.42]; P* = 0.02) and the clinical subject exams (mean 74.01 vs. 78.66; 95% CI [-7.39 to -1.92]; P* < 0.001). When we looked at USMLE performance (Fig. 5), we again found that students who were Age 30 + at matriculation scored significantly lower on both Step 1 (mean 220.8 vs. 231.4; 95% CI [-18.07 to -3.17]; P* = 0.005) and Step 2 CK (mean 234.9^ vs. 247.6^; 95% CI [-22.11 to -3.30]; P^ = 0.01, equal variance NOT assumed). Of note, the statistical analysis of USMLE Step 2 CK performance in this group violated the assumption of equal variances. Nevertheless, the results are included in the figure for transparency and visual continuity.
Results of USMLE performance between students age 30 + vs. under 30 at matriculation. While actual scores can range from 0 to 300, the y-axis has been amended to a range of 215 to 250 in order to visually present the data. Abbreviations: USMLE United States Medical Licensing Examination ^equal variances NOT assumed
Discussion
Academic performance
URM students scored lower, on average, than their non-URM peers on all academic performance measures, with statistically significant lower average performance on the preclinical exams (Figs. 2 and 3; see also Supplementary Table 2, Appendix 2). Although these results were only partially statistically significant, this trend in academic performance among URM students is important because it echoes historic trends in assessment performance disparities impacting racial and ethnic minority students [34,35,36,37,38]. Research on the achievement gap in medical education has highlighted how structural inequities in education, stemming from poorly funded K-12 schools that primarily serve low-income and minority children, lead to disparities in performance on standardized exams, including the Medical College Admission Test (MCAT) and United States Medical Licensing Examinations (USMLE) [34,35,36]. The most recent AAMC report on medical school applicants and matriculants, which included data from the 2022–2023 application cycle, showed that URM students (Black/African American, Hispanic/Latino/Spanish, and American Indian/Alaskan Native/Native Hawaiian/Pacific Islander) had lower average GPAs and MCAT scores than non-URM students [39]. A 2019 study led by a team at the National Board of Medical Examiners (NBME), found that Hispanic and Black students were significantly more likely to score lower on any of the Step exams compared to White students, and that nearly half of all students who initially fail Step 1 are racial/ethnic minority students [37].
Students who were 30 years of age or older at matriculation had significantly lower average exam scores across all academic performance measures compared to their younger counterparts (Figs. 4 and 5; see also Supplementary Table 3, Appendix 2). These findings indicate that there is a need that is not being met for these students. Previous research, though considerably outdated, has suggested that older medical students may have different learning strategies than their younger counterparts. In a 1998 study at McGill University, Feil et. al. found that older medical students approached learning more abstractly, with concern for the thought processes involved in basic and clinical science, while younger students were more inclined to study by memorizing facts for a test for the sake of getting good grades [40]. In 2000, Kick et. al. reported that older students perceived medical school to be more intrusive upon their deeply developed personal lives, and that responsibilities at home made it difficult to study [18]. Given the paucity of recent research on the experiences of older medical students, our findings contribute immensely to the literature. Older medical students bring valuable life experience to patient care and further research to identify factors that may be undermining academic performance among these students is necessary.
Stress
Surprisingly, the only comparison of stress that showed statistically significant higher stress among any of our study groups was between first-generation and continuing-generation college students at the end of third-year clerkships (Fig. 1; see also Supplementary Table 1, Appendix 2). We posit that, because we found evidence of significantly higher perceived stress among only first-generation college students and specifically at the end of third year clerkships, a time when FGCS are exposed to a variety of unfamiliar clinical settings and a highly competitive learning environment, this unique finding may be related to imposter phenomenon.
Imposter phenomenon is characterized by an overwhelming belief that one does not belong in a certain setting despite evidence to the contrary and fear about being discovered as a “fraud” [41]. People experiencing imposter phenomenon have chronic self-doubt and are unable to internalize personal achievements [41]. Levant, et. al. (2020) found significant correlations between stress (measured with the 10-item perceived stress scale [PSS-10]) and imposter feelings (measured with the Clance Impostor Phenomenon Scale), and that PSS-10 scores were 28–31% higher in those experiencing imposter phenomenon [42]. Studies on FGCS at the undergraduate level have shown that these students more frequently report difficulty fitting into campus culture and often doubt their abilities to succeed, feelings that are directly related to imposter syndrome [43, 44]. Canning, et. al. (2019) looked at associations between peer competition, generational status, and imposter feelings in students taking Science, Technology, Engineering, and Mathematics (STEM) undergraduate courses [45]. They found that FGCS were significantly more likely to experience imposter feelings in settings where perceived competition was increased (e.g., STEM courses) [45]. Although further investigation is needed to make a definitive conclusion about the source of the increased stress in this study group, our results parallel that of previous research on the experience of imposter phenomenon among first-generation college students. This theory is further supported by the absence of significant reductions in exam performance among the FGCS in our study, as this provides evidence that these students are not academically inferior to their peers.
Negative findings
In none of the study groups did we find both higher stress and lower academic performance. In fact, our results show that URM and Age 30 + students arrived at medical school with the lowest reported stress of any group (Tables 3 and 6, respectively). Based on socioeconomic disadvantage (SED), no significant differences in stress or academic performance were found. Our lack of any significant differences among SED students compared to their non-SED counterparts, particularly with regards to stress, was surprising, as the association of debt and stress is well-established and existing literature has shown increased stress in these students [1, 13]. Given the sociodemographic diversity of our study participants (Table 1), it would be reasonable to infer that a culture of inclusion and acceptance exists among the students, which may be protective against stress and its sequela.
Additionally, these findings may reflect individual differences in stress appraisal and resilience. Research on stress theory holds that the effects of stress depend, at least in part, on whether the stress is perceived as enhancing or debilitating [46]. For those who perceive stress as enhancing, it can improve performance and enhance motivation to overcome a challenge [46]. Perhaps the FGCS in our study, while they have significantly higher stress than CGCS at the end of third-year clerkships, may be less inclined to appraise stress as a negative factor, and thus academic performance was not impacted. The older students significantly under-performed on all academic measures (Figs. 4 and 5) yet report some of the lowest stress levels of anyone until they approach the residency match (Table 6). Studies on older medical students indicate that they are more likely to hold an internal locus of control, demonstrate greater critical thinking abilities, and have an increased propensity for self-reflection [47, 48]. Having led full lives, with prior careers and other life experience, it is possible the older students approach the burden of medical school differently and may be more accepting of their personal limitations. Moreover, by virtue of their nontraditional sociodemographic backgrounds, these students may possess greater resilience. If our nontraditional students have lived experiences overcoming greater adversity, then they may be less inclined to perceive, or report, increases in stress.
Limitations
Our study has several limitations. Our unusually diverse but small study population involving students from a single institution may limit the generalizability of our results. It is likely that our small sample size contributes to many of our comparisons being found statistically non-significant. Our statistical analysis does not account for students who fall into multiple sociodemographic groups. The collection of program evaluation data by Kirk Kerkorian School of Medicine necessitates that the surveys be a required component of the curriculum. Because of this, it is possible that our results were confounded by individual differences in attention and reflection on the survey questions. While the PSS-4 was designed to be better suited for settings in which respondents may not have the time or desire to complete the longer versions of the PSS (e.g., the 10-item and 14-item questionnaires) [31], and indeed this was the rationale for using the Short Form PSS, it is possible for students to simply click though the survey because it is required to do so without responding thoughtfully to the survey questions. If this is the case, then the survey results would not reflect what we are trying to measure. Lastly, the statistical analysis of differences in USMLE Step 2 CK performance in the “age 30 + ” group violated the assumption of equal variances which remains unexplained by our data set.
Implications
Expanding the sociodemographic diversity among physicians, and by extension, medical students, has long been recognized as fundamental to addressing healthcare inequities in the US [49]. In 2009, the Liaison Committee on Medical Education (LCME) began implementing accreditation standards regarding the benefits of diversity, which now also include policies on anti-discrimination, cultural competency, and addressing disparities in social determinants of health [50,51,52]. Today, considerable effort is put towards increasing the matriculation of students from nontraditional sociodemographic backgrounds. Medical schools have universally adopted holistic admissions policies that recognize socioeconomic status, demographic characteristics, and life experiences of applicants to encourage the matriculation of nontraditional students [24, 53,54,55]. Pipeline programs have been implemented in some areas to recruit students to medicine from community colleges, where many nontraditional students begin their post-secondary education [22,23,24, 36, 56, 57]. Despite these efforts, however, disparities in the availability and quality of healthcare resources, burden of cost, health insurance coverage, patient outcomes, general health status, and overall life expectancy continue to exist for racial/ethnic minority, low-income, and inner city, and rural communities [58].
The purpose of this study was to explore relationships between sociodemographic characteristics, stress, and academic performance, in the context of outcomes that may be undermining efforts to diversify the physician workforce. Nontraditional students bring to medicine inherent characteristics and perspectives that enrich the learning environment [21], and contribute to expanding access to culturally competent, linguistically appropriate healthcare services for underserved communities in the US [22,23,24]. With a projected shortage of up to 124,000 physicians by 2034 [59], and the significant lag time between embarking on post-secondary education and independent practice, increasing the diversity among medical students is more urgent than ever. Results from our study suggest that aspects of medical education are unfavorable and disadvantageous for first-generation, URM and older medical students. Residency program directors continue to use USMLE test scores as a primary metric to screen applicants [60]. Therefore, poor performance on these exams has profound consequences on career trajectory which, in turn, may be impeding progress towards increasing diversity in medicine. The increased stress in first-generation students at the end of third year clerkships may be indicative of underlying psychological distress.
A deeper understanding of the interplay between sociodemographic characteristics and success in medical school, both psychosocially and academically, is paramount if we are to achieve diversity in medicine that matches that of the population and, ultimately, health equity. Our study looked at stress, which is just one possible cause for nontraditional students to be unsuccessful in medical school, and we looked at academic performance, which is just one possible measure of success or failure in medical school. The PSS-4 captures general stress at moments in time, but it tells us nothing about the quality of stress. Further investigation employing qualitative methods could elucidate sources of stress and factors undermining academic performance for nontraditional students. While USMLE exam performance continues to be a critical component of a student’s competitiveness for residency programs, it is closely followed by narrative evaluations [60]. Moreover, there is evidence that narrative evaluations, which are inherently subjective, are prone to both implicit and explicit bias, thereby adding another element of disadvantage for certain groups of nontraditional students [35, 61, 62]. To fully understand the experience of nontraditional medical students, exploring the effect of these evaluations, both internally at our institution and broadly across the US, is necessary. It is incumbent upon medical educators to support their students in meaningful ways and to promote the success of nontraditional students. This may be through individualized support, both academically and personally, flexible curricula to meet the needs of a diverse student body, or through system-level changes that lead to learning environments more favorable to nontraditional students.
Conclusion
Results from our study echo historic trends in academic performance for racial and ethnic minority students, with our URM students scoring significantly lower on the standardized preclinical NBME exams than their non-URM peers. Additionally, we present recent evidence of academic performance disparities based on age at matriculation, with our Age 30 + study group significantly underperforming on both institutional exams and national licensing exams. Our results also show significantly higher stress at the end of the third year of medical school for first-generation students, which may be evidence of imposter phenomenon, though further investigation is needed to make that conclusion definitively. Contrary to the literature, however, we did not find any differences based on socioeconomic disadvantage; we attribute this inconsistency to limitations imparted on our study by the nature of the study design itself.
Availability of data and materials
Data available upon request. Please send data requests to Edward Simanton PhD, edward.simanton@unlv.edu.
Notes
Nontraditional student refers to students who are considered first-generation college students, underrepresented in medicine minority, socioeconomically disadvantaged, or took any path to medical school other than completing high school, then completing a bachelor’s degree 4 years later, then immediately matriculating to medical school.
Abbreviations
- USMLE:
-
United States Medical Licensing Examination
- URM:
-
Underrepresented in medicine
- NCHA:
-
National College Health Assessment
- PSS:
-
Perceived Stress Scale
- IRB:
-
Internal review board
- FGCS:
-
First-generation college student
- URM:
-
Underrepresented in medicine
- SED:
-
Socioeconomically Disadvantaged
- AAMC:
-
Association of American Medical Colleges
- US:
-
United States
- CGCS:
-
Continuing-generation college students
- SES:
-
Socioeconomic status
- EO:
-
Education-Occupation
- SES-EO:
-
Socioeconomic Status-Education Occupation
- MSQ:
-
Matriculating Student Questionnaire
- PSS-4:
-
Perceived Stress Scale-4 (short form)
- NBME:
-
National Board of Medical Examiners
- USMLE:
-
United States Medical Licensing Examination
- CK:
-
Clinical Knowledge
- SPSS:
-
Statistical Package for Social Sciences
- FGCS:
-
First-generation college student
- CGCS:
-
Continuing-generation college student
- URM:
-
Underrepresented in medicine
- PSS-4:
-
Perceived Stress Scale-4 (short form)
- SED:
-
Socioeconomic disadvantage
- USMLE:
-
United States Medical Licensing Examination
- Step 2 CK:
-
Step 2 Clinical Knowledge
- CI:
-
Confidence interval
- URM:
-
Underrepresented in medicine
- MCAT:
-
Medical College Admission Test
- USMLE:
-
United States Medical Licensing Examination
- AAMC:
-
Association of American Medical Colleges
- GPA:
-
Grade-point average
- NBME:
-
National Board of Medical Examiners
- FGCS:
-
First-generation college student
- PSS-10:
-
Perceived Stress Scale-10 (10-item questionnaire)
- STEM:
-
Science, technology, engineering, and mathematics
- SED:
-
Socioeconomic disadvantage
- CGCS:
-
Continuing-generation college students
- PSS-4:
-
Perceived Stress Scale-4 (short form)
- LCME:
-
Liaison Committee on Medical Education
- US:
-
United States
- URM:
-
Underrepresented in medicine
- NBME:
-
National Board of Medical Examiners
References
Pisaniello MS, Asahina AT, Bacchi S, Wagner M, Perry SW, Wong M, Licinio J. Effect of medical student debt on mental health, academic performance and specialty choice: a systematic review. BMJ Open. 2019;9(7):e029980. https://0-doi-org.brum.beds.ac.uk/10.1136/bmjopen-2019-029980.
McKerrow I, Carney PA, Caretta-Weyer H, Furnari M, Miller Juve A. Trends in medical students’ stress, physical, and emotional health throughout training. Medical Education Online. 2020;25(1):1709278. https://0-doi-org.brum.beds.ac.uk/10.1080/10872981.2019.1709278.https://0-www-tandfonline-com.brum.beds.ac.uk/doi/abs/10.1080/10872981.2019.1709278.
Rajapuram N, Langness S, Marshall MR, Sammann A. Medical students in distress: The impact of gender, race, debt, and disability. PloS One. 2020;15(12):e0243250. https://0-doi-org.brum.beds.ac.uk/10.1371/journal.pone.0243250.https://0-www-ncbi-nlm-nih-gov.brum.beds.ac.uk/pubmed/33270759.
Dyrbye LN, West CP, Satele D, Boone S, Tan L, Sloan J, Shanafelt TD. Burnout Among U.S. Medical Students, Residents, and Early Career Physicians Relative to the General U.S. Population. Academic medicine. 2014;89(3):443–51. https://0-doi-org.brum.beds.ac.uk/10.1097/ACM.0000000000000134. https://0-www-ncbi-nlm-nih-gov.brum.beds.ac.uk/pubmed/24448053.
Dyrbye L, Shanafelt T. A narrative review on burnout experienced by medical students and residents. Med Educ. 2016;50(1):132–49. https://0-doi-org.brum.beds.ac.uk/10.1097/ACM.0000000000000134. https://0-doi-org.brum.beds.ac.uk/10.1111/medu.12927.
Harolds JA. Quality and Safety in Healthcare, Part LXVI: Contributing Causes of Poor Well-being in Medical Students. Clin Nucl Med. 2021;46(2):133–5. https://0-doi-org.brum.beds.ac.uk/10.1097/RLU.0000000000002969.https://0-www-ncbi-nlm-nih-gov.brum.beds.ac.uk/pubmed/32108702.
Committee on Systems Approaches to Improve Patient Care by Supporting Clinician Well-Being, National Academy of Medicine, National Academy of Sciences, Engineering, and Medicine: Taking action against clinician burnout : a systems approach to professional well-being: Washington, DC: The National Academies Press; 2019. https://0-doi-org.brum.beds.ac.uk/10.17226/25521.
American College Health Association: ACHA-NCHA III: Graduate/Professional Student Reference Group Executive Summary Spring 2022. American College Health Association. 2022, https://www.acha.org/NCHA/ACHA-NCHA_Data/Publications_and_Reports/NCHA/Data/Reports_ACHA-NCHAIII.aspx.
Hill MR, Goicochea S, Merlo LJ. In their own words: stressors facing medical students in the millennial generation. Med Edu Online. 2018;23(1):1530558–10. https://0-doi-org.brum.beds.ac.uk/10.1080/10872981.2018.1530558.https://0-www-tandfonline-com.brum.beds.ac.uk/doi/abs/10.1080/10872981.2018.1530558.
Dyrbye LN, Thomas MR, Shanafelt TD. Systematic review of depression, anxiety, and other indicators of psychological distress among U.S. and Canadian medical students. Acad Med. 2006;81(4):354–73. https://0-doi-org.brum.beds.ac.uk/10.1097/00001888-200604000-00009.https://0-www-ncbi-nlm-nih-gov.brum.beds.ac.uk/pubmed/16565188.
Dyrbye LN, Sciolla AF, Dekhtyar M, Rajasekaran S, Allgood JA, Rea M, Knight AP, Haywood A, Smith S, Stephens MB. Medical school strategies to address student well-being: a national survey. Acad Med. 2019;94(6):861–8. https://0-doi-org.brum.beds.ac.uk/10.1097/ACM.0000000000002611.https://0-www-ncbi-nlm-nih-gov.brum.beds.ac.uk/pubmed/30681453.
Kligler B, Linde B, Katz NT. Becoming a doctor: a qualitative evaluation of challenges and opportunities in medical student wellness during the third year. Acad Med. 2013;88(4):535–40. https://0-doi-org.brum.beds.ac.uk/10.1097/ACM.0b013e3182860e6d.https://0-www-ncbi-nlm-nih-gov.brum.beds.ac.uk/pubmed/23425993.
McMichael B, Lee A IV, Fallon B, Matusko N, Sandhu G. Racial and socioeconomic inequity in the financial stress of medical school. MedEdPublish. 2022;12:3. https://0-doi-org.brum.beds.ac.uk/10.12688/mep.17544.2.https://0-search-proquest-com.brum.beds.ac.uk/docview/2718963370.
Amirkhan JH, Manalo R, Velasco SE: Stress overload in first-generation college students: Implications for intervention. Psychol Serv. 2022:1–11. https://0-doi-org.brum.beds.ac.uk/10.1037/ser0000650 Advance online publication(-). https://0-www-ncbi-nlm-nih-gov.brum.beds.ac.uk/pubmed/35389674.
Mason HRC, Winseman J, Marcellon R, Huamantl M, Ruiz C, Ayala EE. First-Generation medical student wellness in the United States. J Best Pract Health Prof Divers. 2018;11(2):96–106 (https://0-www-jstor-org.brum.beds.ac.uk/stable/26894211).
Stevens C, Liu CH, Chen JA. Racial/ethnic disparities in US college students’ experience: Discrimination as an impediment to academic performance. J Am Coll Health. 2018;66(7):665–73. https://0-doi-org.brum.beds.ac.uk/10.1080/07448481.2018.1452745.
Smedley BD, Myers HF, Harrell SP. Minority-status stresses and the college adjustment of ethnic minority freshmen. J Higher Educ. 1993;64(4):434–52. https://0-doi-org.brum.beds.ac.uk/10.1080/00221546.1993.11778438.https://0-www-tandfonline-com.brum.beds.ac.uk/doi/abs/10.1080/00221546.1993.11778438.
Kick S, Adams L, O’Brien-Gonzales A. Unique Issues of Older Medical Students. Teach Learn Med. 2000;12(3):150–5. https://0-doi-org.brum.beds.ac.uk/10.1207/S15328015TLM1203_6.
Furquim F, Glasener KM, Oster M, McCall BP, DesJardins SL. Navigating the Financial Aid Process: Borrowing Outcomes among First-Generation and Non-First-Generation Students. Ann Am Acad Polit SS. 2017;671(1):69–91. https://0-doi-org.brum.beds.ac.uk/10.1177/0002716217698119.https://0-doi-org.brum.beds.ac.uk/10.1177/0002716217698119.
Grayson MS, Newton DA, Thompson LF. Payback time: the associations of debt and income with medical student career choice. Med Educ. 2012;46(10):983–91. https://0-doi-org.brum.beds.ac.uk/10.1111/j.1365-2923.2012.04340.x.https://api.istex.fr/ark:/67375/WNG-MFLPNPP3-4/fulltext.pdf.
Thomas BR, Dockter N. Affirmative action and holistic review in medical school admissions: where we have been and where we are going. Acad Med. 2019;94(4):473–6. https://0-doi-org.brum.beds.ac.uk/10.1097/ACM.0000000000002482.https://0-www-ncbi-nlm-nih-gov.brum.beds.ac.uk/pubmed/30277960.
Walker KO, Moreno G, Grumbach K. The association among specialty, race, ethnicity, and practice location among California physicians in diverse specialties. J Natl Med Assoc. 2012;104(1):46–52. https://0-doi-org.brum.beds.ac.uk/10.1016/S0027-9684(15)30126-7.https://www.clinicalkey.es/playcontent/1-s2.0-S0027968415301267.
Garcia AN, Kuo T, Arangua L, Pérez-Stable EJ. Factors associated with medical school graduates’ intention to work with underserved populations: policy implications for advancing workforce diversity. Acad Med. 2018;93(1):82–9. https://0-doi-org.brum.beds.ac.uk/10.1097/ACM.0000000000001917.https://0-www-ncbi-nlm-nih-gov.brum.beds.ac.uk/pubmed/28930761.
Association of American Medical Colleges: A Healthier Future for All: The AAMC Strategic Plan. Association of American Medical Colleges; 2023. https://www.aamc.org/about-us/strategic-plan/healthier-future-all-aamc-strategic-plan.
Association of American Medical Colleges: Table A-26: First Generation Applicants, Acceptees, and Matriculants to U.S. MD-Granting Medical Schools, Academic Years 2020-2021 through 2022-2023. AAMC. AAMC 2022, https://www.aamc.org/data-reports/students-residents/data/2022-facts-applicants-and-matriculants-data.
Association of American Medical Colleges: Table A-14.3: Race/Ethnicity Responses (Alone and In Combination) of Matriculants to U.S. MD-Granting Medical Schools, 2019–2020 through 2023–2024. AAMC 2023, . https://www.aamc.org/media/8826/download.
Association of American Medical Colleges: Table A-24: Applicants, Acceptees, and Matriculants to U.S. MD-Granting Medical Schools by Socioeconomic Status (SES), Academic Years 2018–2019 through 2022–2023. AAMC 2022, . https://www.aamc.org/media/57171/download.
Association of American Medical Colleges: Matriculating Student Questionnaire: 2022 All Schools Summary Report. AAMC. 2022, https://www.aamc.org/data-reports/students-residents/report/matriculating-student-questionnaire-msq.
Youngclaus J, Roskovensky L. Analysis in Brief: an updated look at the economic diversity of US medical students. AAMC. 2018;18(5):1–3.https://www.aamc.org/data-reports/analysis-brief/report/updated-look-economic-diversity-us-medical-students.
Association of American Medical Colleges: Underrepresented in medicine definition. (n.d.)., https://www.aamc.org/what-we-do/equity-diversity-inclusion/underrepresented-in-medicine. Accessed 30 Oct 2022.
Warttig SL, Forshaw MJ, South J, White AK. New, normative, English-sample data for the Short Form Perceived Stress Scale (PSS-4). J Health Psychol. 2013;18(12):1617–28. https://0-doi-org.brum.beds.ac.uk/10.1177/1359105313508346.
Cohen S, Kamarck T, Mermelstein R. A Global Measure of Perceived Stress. J Health Soc Behav. 1983;24(4):385–96. https://0-doi-org.brum.beds.ac.uk/10.2307/2136404.https://0-www-jstor-org.brum.beds.ac.uk/stable/2136404.
Association of American Medical Colleges: Medical School Year Two Questionnaire: 2022 All Schools Summary Report. AAMC. 2022, https://www.aamc.org/data-reports/students-residents/report/year-two-questionnaire-y2q.
Jones AC, Nichols AC, McNicholas CM, Stanford FC. Admissions is not enough: the racial achievement gap in medical education. Acad Med. 2021;96(2):176–81. https://0-doi-org.brum.beds.ac.uk/10.1097/ACM.0000000000003837.
Teherani A, Hauer KE, Fernandez A, King TE, Lucey C. How small differences in assessed clinical performance amplify to large differences in grades and awards: a cascade with serious consequences for students underrepresented in medicine. Acad Med. 2018;93(9):1286–92. https://0-doi-org.brum.beds.ac.uk/10.1097/ACM.0000000000002323.https://0-www-ncbi-nlm-nih-gov.brum.beds.ac.uk/pubmed/29923892.
Poll-Hunter NI, Brown Z, Smith A, Starks SM, Gregory-Bass R, Robinson D, Cullins MD, Capers Q, Landry A, Bush A, Bellamy K, Lubin-Johnson N, Fluker CJ, Acosta DA, Young GH, Butts GC, Bright CM. Increasing the representation of black men in medicine by addressing systems factors. Acad Med. 2023;98(3):304–12. https://0-doi-org.brum.beds.ac.uk/10.1097/ACM.0000000000005070.https://0-www-ncbi-nlm-nih-gov.brum.beds.ac.uk/pubmed/36538673.
Rubright JD, Jodoin M, Barone MA. Examining demographics, prior academic performance, and United States medical licensing examination scores. Acad Med. 2019;94(3):364–70. https://0-doi-org.brum.beds.ac.uk/10.1097/ACM.0000000000002366.https://0-www-ncbi-nlm-nih-gov.brum.beds.ac.uk/pubmed/30024473.
Andriole DA, Jeffe DB. A National Cohort Study of U.S. Medical School Students Who Initially Failed Step 1 of the United States Medical Licensing Examination. Academic medicine. 2012;87(4):529–36. https://0-doi-org.brum.beds.ac.uk/10.1097/ACM.0b013e318248dd9c.https://0-www-ncbi-nlm-nih-gov.brum.beds.ac.uk/pubmed/22361789.
Association of American Medical Colleges: Table A-18: MCAT Scores and GPAs for Applicants and Matriculants to U.S. MD-Granting Medical Schools by Race/Ethnicity, 2022–2023. AAMC. AAMC 2022, https://www.aamc.org/media/6066/download
Feil D, Kristian M, Mitchell N. Older medical students’ performances at McGill University. Acad Med. 1998;73(1):98–100. https://0-doi-org.brum.beds.ac.uk/10.1097/00001888-199801000-00020.
Villwock JA, Sobin LB, Koester LA, Harris TM. Impostor syndrome and burnout among American medical students: a pilot study. Int J Med Educ. 2016;7:364–9. https://0-doi-org.brum.beds.ac.uk/10.5116/ijme.5801.eac4.https://0-www-ncbi-nlm-nih-gov.brum.beds.ac.uk/pubmed/27802178.
Levant B, Villwock JA, Manzardo AM. Impostorism in American medical students during early clinical training: gender differences and intercorrelating factors. Int J Med Educ. 2020;11:90–6. https://0-doi-org.brum.beds.ac.uk/10.5116/ijme.5e99.7aa2.
Pratt IS, Harwood HB, Cavazos JT, Ditzfeld CP. Should I Stay or Should I Go? Retention in First-Generation College Students. J Coll Stud Retent Re Theory Pract. 2019;21(1):105–18. https://0-doi-org.brum.beds.ac.uk/10.1177/1521025117690868.https://0-journals-sagepub-com.brum.beds.ac.uk/doi/full/10.1177/1521025117690868.
Stebleton M, Soria K. Breaking down barriers: Academic obstacles of first-generation students at research universities. Learn Assist Rev. 2013;17(2):8–20.https://eric.ed.gov/?id=EJ1002281.
Canning EA, LaCosse J, Kroeper KM, Murphy MC. Feeling like an imposter: the effect of perceived classroom competition on the daily psychological experiences of first-generation college students. Soc Psychol Pers Sci. 2020;11(5):647–57. https://0-doi-org.brum.beds.ac.uk/10.1177/1948550619882032.
Crum AJ, Salovey P, Achor S. Rethinking Stress: The Role of Mindsets in Determining the Stress Response. J Pers Soc Psychol. 2013;104(4):716–33. https://0-doi-org.brum.beds.ac.uk/10.1037/a0031201.http://psycnet.apa.org/journals/psp/104/4/716.
Goldie J. The formation of professional identity in medical students: Considerations for educators. Med Teach. 2012;34(9):e641–8. https://0-doi-org.brum.beds.ac.uk/10.3109/0142159X.2012.687476.
Matthews R, Smith-Han K, Nicholson H. From physiotherapy to the army: negotiating previously developed professional identities in mature medical students. Adv in Health Sci Educ. 2020;25(3):607–27. https://0-doi-org.brum.beds.ac.uk/10.1007/s10459-019-09942-0.
Cohen JJ, Gabriel BA, Terrell C. The case for diversity in the health care workforce. Health Affairs. 2002;21(5):90–102. https://0-doi-org.brum.beds.ac.uk/10.1377/hlthaff.21.5.90.http://content.healthaffairs.org/cgi/content/abstract/21/5/90.
Boatright DH, Samuels EA, Cramer L, Cross J, Desai M, Latimore D, Gross CP. Association between the liaison committee on medical education’s diversity standards and changes in percentage of medical student sex, race, and ethnicity. JAMA. 2018;320(21):2267–9. https://0-doi-org.brum.beds.ac.uk/10.1001/jama.2018.13705.
Association of American Medical Colleges: Liaison Committee on Medical Education (LCME) Standards on Diversity. 2009, https://health.usf.edu/~/media/Files/Medicine/MD%20Program/Diversity/LCMEStandardsonDiversity1.ashx?la=en.
Liaison Committee on Medical Education: Functions and Structure of a Medical School. AAMC 2023, . https://lcme.org/publications/.
Grbic D, Morrison E, Sondheimer HM, Conrad SS, Milem JF. The Association between a holistic review in admissions workshop and the diversity of accepted applicants and students matriculating to medical school. Academic medicine. 2019;94(3):396–403. https://0-doi-org.brum.beds.ac.uk/10.1097/ACM.0000000000002446.https://0-www-ncbi-nlm-nih-gov.brum.beds.ac.uk/pubmed/30188373.
Bright CM, Price MA, Morgan RC, Bailey RK. The Report of the W. Montague Cobb /NMA Health Institute Consensus Panel on the Plight of Underrepresented Minorities in Medical Education. J Natl Med Assoc. 2018;110(6):614–23. https://0-doi-org.brum.beds.ac.uk/10.1016/j.jnma.2018.03.012.https://0-www-proquest-com.brum.beds.ac.uk/scholarly-journals/report-w-montague-cobb-nma-health-institute/docview/2188190276/se-2?accountid=3611.
Dandar V, Fair M, Steinecke A, Sweeny N, Mallory T: The Power of Collective Action: Assessing and Advancing Diversity, Equity, and Inclusion Efforts at AAMC Medical Schools. AAMC 2022, https://www.aamc.org/data-reports/report/assessing-and-advancing-dei-efforts-aamc-medical-schools.
Talamantes E, Jerant A, Henderson MC, Griffin E, Fancher T, Grbic D, Moreno G, Franks P. Community college pathways to medical school and family medicine residency training. Ann Family Med. 2018;16(4):302–7. https://0-doi-org.brum.beds.ac.uk/10.1370/afm.2270.https://www.clinicalkey.es/playcontent/1-s2.0-S1544170919300071.
Ma J, Baum S: Research on the Student-centered Talent Cultivation in Universities and Colleges. Atlantis Press; 2016. https://0-doi-org.brum.beds.ac.uk/10.2991/icessms-16.2017.111.
Agency for Healthcare Research and Quality: 2022 National Healthcare Quality and Disparities Report. U.S. Department of Health and Human Services. U.S. Department of Health and Human Services 2022, 22(23)-0030 https://www.ahrq.gov/sites/default/files/wysiwyg/research/findings/nhqrdr/2022qdr-final-es.pdf.
Reynolds R, Ritashree Chakrabarti, Chylak D, Jones K, Iacobucci W, Dall T: The Complexities of Physician Supply and Demand: Projections From 2019 to 2034. IHS Markit Ltd. & AAMC. IHS Markit Ltd. 2021, https://www.search.datacite.org/works/10.13140/rg.2.2.29404.92808.
National Resident Matching Program Data Release and Research Committee: Results of the 2021 NRMP Program Director Survey. National Resident Matching Program. National Resident Matching Program 2021, https://www.nrmp.org/wp-content/uploads/2021/11/2021-PD-Survey-Report-for-WWW.pdf.
Rojek AE, Khanna R, Yim JWL, Gardner R, Lisker S, Hauer KE, Lucey C, Sarkar U. Differences in Narrative Language in Evaluations of Medical Students by Gender and Under-represented Minority Status. J Gen Intern Med. 2019;34(5):684–91. https://0-doi-org.brum.beds.ac.uk/10.1007/s11606-019-04889-9.https://0-link-springer-com.brum.beds.ac.uk/article/10.1007/s11606-019-04889-9.
Low D, Pollack SW, Liao ZC, Maestas R, Kirven LE, Eacker AM, Morales LS. Racial/Ethnic disparities in clinical grading in medical school. Teach Learn Med. 2019;31(5):487–96. https://0-doi-org.brum.beds.ac.uk/10.1080/10401334.2019.1597724.https://0-www-tandfonline-com.brum.beds.ac.uk/doi/abs/10.1080/10401334.2019.1597724.
Acknowledgements
The authors would like to thank Dr. Dale Netski, Director of Medical Student Research, for his review of the manuscript, and Kathryn M. Houk, Undergraduate Medical Education Librarian, for her assistance with resource utilization and citation management software.
Funding
No funding was accepted to assist with this study or preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
DE made substantial contributions to literature review, methods conception, data analysis, preparation and revision of all parts of the manuscript. ST made substantial contributions to literature review, data analysis, discussion, conclusion, review and editing of all parts of the manuscript. KN made substantial contributions to literature review, data analysis, and editing of all parts of the manuscript. ES made substantial contributions to methods conception, data retrieval from institutional databases, data analysis, review and editing of all parts of the manuscript. AW made substantial contributions to methods conception, data analysis, review and editing of all parts of the manuscript. All authors reviewed and approved the final version of this manuscript.
Authors’ information
DE is a medical student at the Kirk Kerkorian School of Medicine at UNLV, graduating May 2024.
ST is a medical student at the Kirk Kerkorian School of Medicine at UNLV, graduating May 2024.
KN is a medical student at the Kirk Kerkorian School of Medicine at UNLV, graduating May 2026.
ES is Director of Educational Outcomes and Assessment at Kirk Kerkorian School of Medicine at UNLV.
AW is Director of Well-Being & Integrative Medicine and Associate Professor of Medical Education at Kirk Kerkorian School of Medicine at UNLV.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Biomedical Institutional Review Board of the University of Nevada Las Vegas. All experimental protocols, including waiver of informed consent, were approved by the Biomedical Institutional Review Board of the University of Nevada Las Vegas ethics committee. All methods were carried out in accordance with relevant guidelines and regulations and in accordance with the IRB-approved protocol “School of Medicine use of program evaluation data for research” [protocol number 1030906–1], dated April 3rd, 2017.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Eames, D., Thomas, S., Norman, K. et al. Sociodemographic disadvantage in the burden of stress and academic performance in medical school: implications for diversity in medicine. BMC Med Educ 24, 348 (2024). https://0-doi-org.brum.beds.ac.uk/10.1186/s12909-024-05263-y
Received:
Accepted:
Published:
DOI: https://0-doi-org.brum.beds.ac.uk/10.1186/s12909-024-05263-y